(A Practical, Evidence-Based Guide for Indian Urologists)
Prostate cancer diagnosis has evolved dramatically over the last decade. For many years, multiparametric MRI (mpMRI) became the preferred imaging tool before biopsy. Recently, micro-ultrasound—particularly the ExactVu™ 29 MHz platform—has transformed how urologists visualize and target prostate lesions in real time.
This has led to one of the most common questions urologists ask today:
“Micro-ultrasound or MRI — which is better for diagnosing prostate cancer?”
In this article, we break down the differences, strengths, limitations, and practical advantages of each technology. Our goal is simple: provide a clear, real-world answer that helps clinicians choose the right modality for their practice.
Understanding the Two Technologies
1.Multiparametric MRI (mpMRI)
MRI uses T2, diffusion-weighted imaging (DWI/ADC), and dynamic contrast sequences to identify suspicious prostate lesions. Reporting follows PI-RADS (Prostate Imaging – Reporting & Data System).
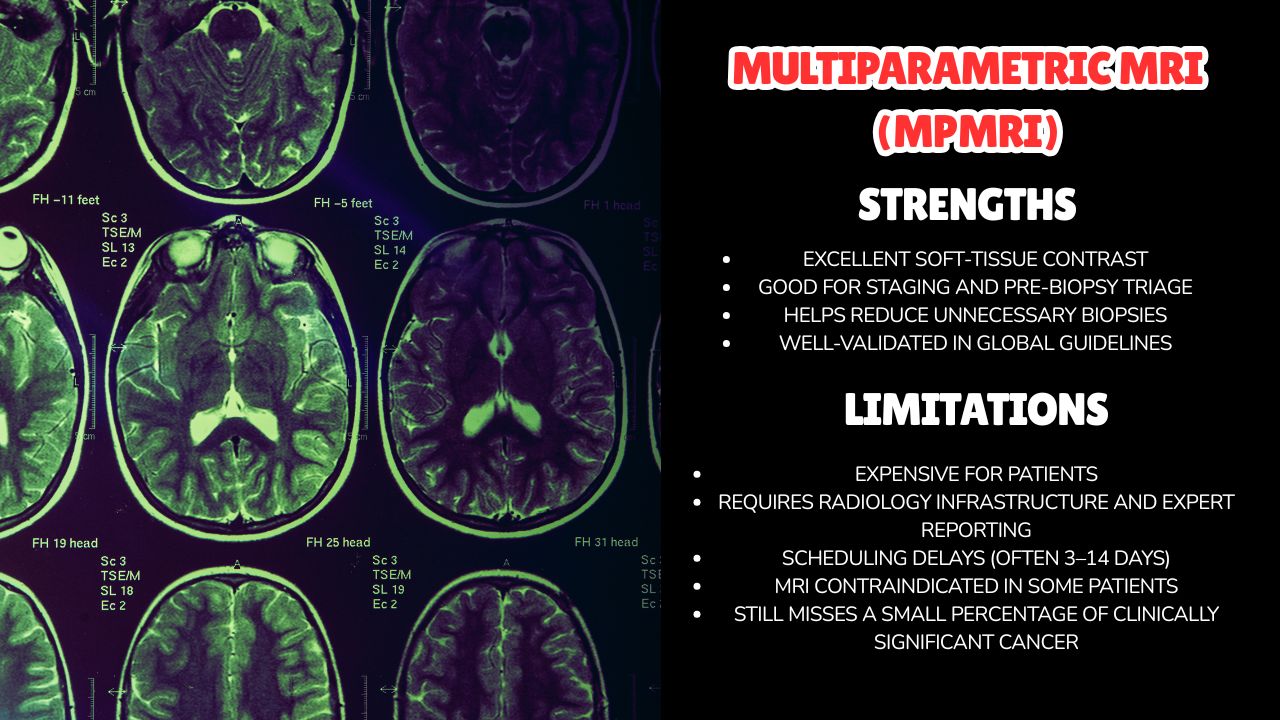
Strengths
- Excellent soft-tissue contrast
- Good for staging and pre-biopsy triage
- Helps reduce unnecessary biopsies
- Well-validated in global guidelines
Limitations
- Expensive for patients
- Requires radiology infrastructure and expert reporting
- Scheduling delays (often 3–14 days)
- MRI contraindicated in some patients
- Still misses a small percentage of clinically significant cancer
2.Micro-Ultrasound (ExactVu™ 29 MHz)
Micro-ultrasound delivers high-resolution, real-time imaging at 29 MHz—almost 3× higher resolution than conventional ultrasound. It uses the PRI-MUS scoring system, similar to PI-RADS, to classify lesion risk.
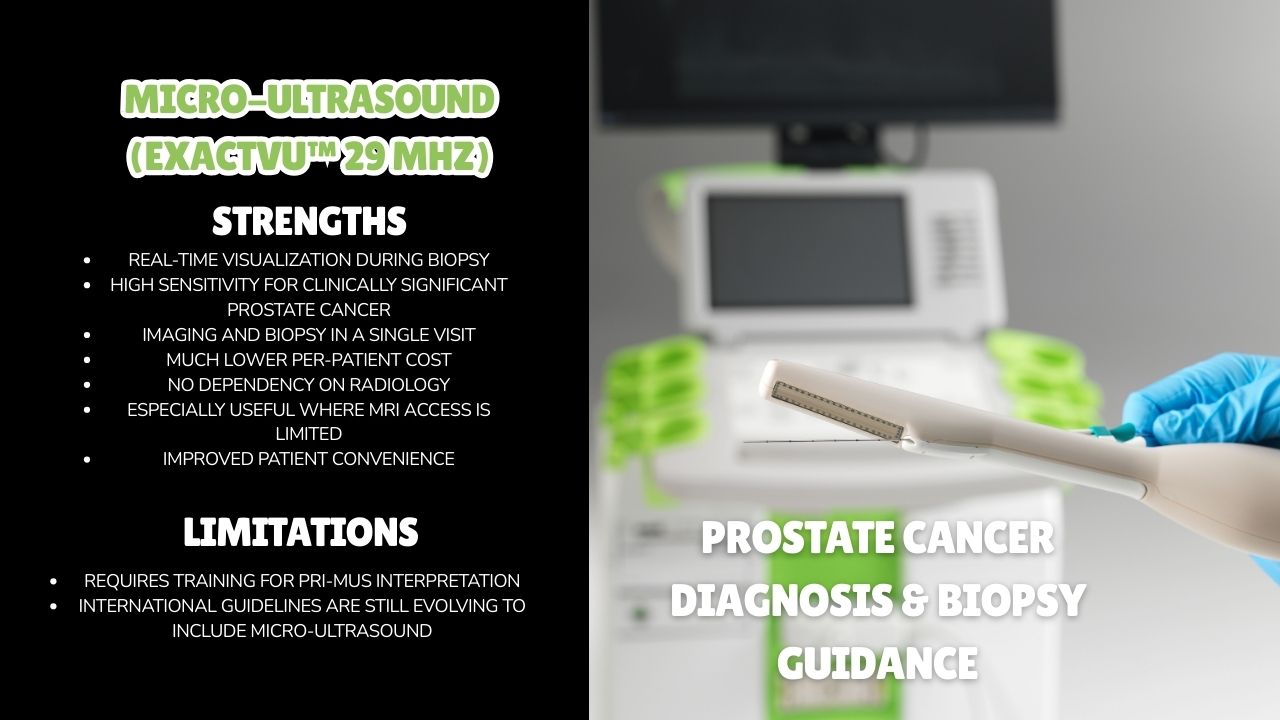
Strengths
- Real-time visualization during biopsy
- High sensitivity for clinically significant prostate cancer
- Imaging and biopsy in a single visit
- Much lower per-patient cost
- No dependency on radiology
- Especially useful where MRI access is limited
- Improved patient convenience
Limitations
- Requires training for PRI-MUS interpretation
- International guidelines are still evolving to include micro-ultrasound
Micro-Ultrasound vs MRI: What Does Clinical Evidence Say?
Multiple studies and systematic reviews have shown:
⭐ 1. Micro-ultrasound detects clinically significant prostate cancer at rates comparable to mpMRI
Meaning: Both modalities perform similarly when the goal is identifying cancer that actually matters.
⭐ 2. Each modality sometimes detects lesions the other misses
This is important. It means:
- MRI finds some lesions that micro-US may not highlight.
- Micro-US finds some lesions that MRI does not detect.
This has led many experts to recommend using both whenever feasible—MRI for planning, micro-US for real-time targeting.
⭐ 3. Micro-ultrasound is more practical in high-volume or resource-limited settings
MRI may not always be fast or affordable for every patient. Micro-US solves this challenge.
Workflow Comparison (Real-World Practice)
MRI Pathway
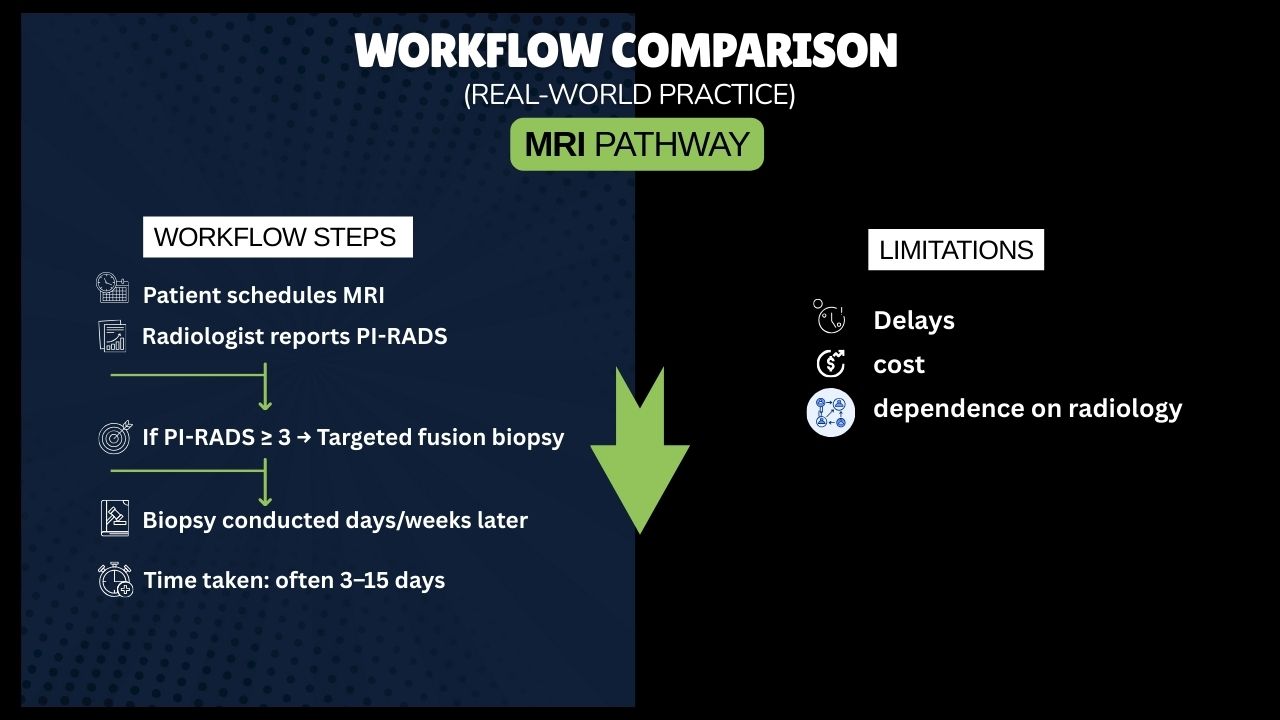
- Patient schedules MRI
- Radiologist reports PI-RADS
- If PI-RADS ≥ 3 → Targeted fusion biopsy
- Biopsy conducted days/weeks later
- Time taken: often 3–15 days
Limit: Delays, cost, dependence on radiology
Micro-Ultrasound Pathway
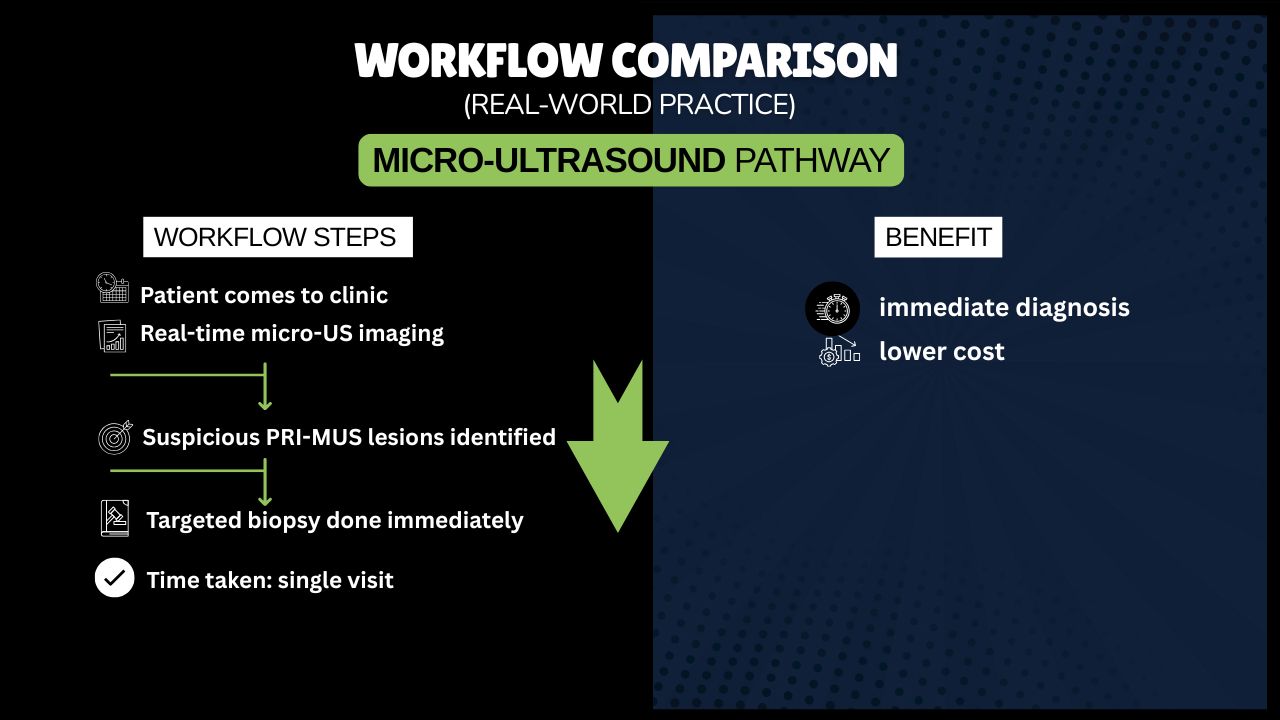
- Patient comes to clinic
- Real-time micro-US imaging
- Suspicious PRI-MUS lesions identified
- Targeted biopsy done immediately
- Time taken: single visit
Benefit: immediate diagnosis, lower cost
Which Should Urologists Use — MRI or Micro-Ultrasound?
Here is the clear, practical answer.
✔ If MRI is easily available and affordable
- Use mpMRI as the triage test, then perform biopsy guided by micro-US or fusion.
- MRI helps plan the biopsy; micro-US improves targeting during the procedure.
✔ If MRI is delayed, expensive, unavailable, or contraindicated
- Use ExactVu Micro-Ultrasound as the primary diagnostic tool.
- It provides MRI-like resolution, real-time imaging, and immediate biopsy capability.
✔ The Most Powerful Approach
- MRI + Micro-Ultrasound Combination
This approach provides:
- Highest sensitivity
- Best lesion localization
- Reduced risk of missing clinically significant cancer
- Best workflow for urologists
Many international centers are moving toward this hybrid model.
Indian Healthcare Reality: The Practical Choice
In India, patients often face:
- MRI cost constraints
- Access issues in Tier 2/3 cities
- Scheduling delays
- Limited radiology specialists
Given these realities, micro-ultrasound offers superior practicality, affordability, and workflow efficiency.
This is why micro-ultrasound—especially ExactVu™—is rapidly being adopted in India as the frontline prostate imaging platform.
Conclusion: The Right Tool Depends on Your Setting
If MRI is available:
→ Use MRI for triage + Micro-US for targeted biopsy
If MRI is not feasible:
→ Micro-Ultrasound alone provides highly reliable diagnosis
If you want maximum accuracy and efficiency:
→ Combine both modalities
ExactVu Micro-Ultrasound is the most adaptable, real-time, cost-effective diagnostic platform for prostate cancer—especially for Indian clinical practice.
About Wellnect India
Wellnect India is the authorized distributor of ExactVu™ Micro-Ultrasound in India.
We support hospitals, uro-centers, and diagnostic facilities with:
- Complete system setup
- Clinical training
- Installation & service support
- Workflow integration guidance
For inquiries or demonstrations:
📞 [+91 88600 86233, +91 99986 91413]
📧 [digitalwellnect@gmail.com]
🌐 www.wellnect.in
Dr abhishek Singh